Monday
This is from the BBC
Tea and coffee drinkers have a lower risk of developing type 2 diabetes, a large body of evidence shows.
And the protection may not be down to caffeine since decaf coffee has the greatest effect, say researchers in Archives of Internal Medicine.
They looked at 18 separate studies involving nearly 500,000 people.
This analysis revealed that people who drink three or four cups of coffee or tea a day cut their risk by a fifth or more, say researchers.
The same amount of decaffeinated coffee had an even bigger effect, lowering risk by a third.
Type 2 diabetes usually starts after the age of 40 and develops when the body can still make some insulin, but not enough, or when the insulin that is produced does not work properly. Type 2 diabetes is treated with a healthy diet and increased physical activity. In addition to this, medication and/or insulin is often required.
The identification of the active components of these beverages would open up new therapeutic pathways for the primary prevention of diabetes mellitus
The study authors
If the findings prove true, doctors may well start advising people to put the kettle on as well as take more exercise and watch their weight, say the researchers.
When the authors combined and analysed the data, they found that each additional cup of coffee consumed in a day cut diabetes risk by 7%.
Lead researcher Dr Rachel Huxley, from the University of Sydney in Australia, said because of the finding with decaffeinated coffee, the link is unlikely to be solely related to caffeine.
Instead, other compounds in coffee and tea - including magnesium and antioxidants known as lignans or chlorogenic acids - may be involved.
Special brew
"The identification of the active components of these beverages would open up new therapeutic pathways for the primary prevention of diabetes mellitus.
"If such beneficial effects were observed in interventional trials to be real, the implications for the millions of individuals who have diabetes mellitus, or who are at future risk of developing it, would be substantial."
Dr Victoria King, of Diabetes UK, said: "Without full information about what other factors may be influencing the type 2 diabetes risk of the studies' participants - such as their physical activity levels and diet - as well as what the active ingredient in tea or coffee appears to be, we cannot be sure what, if anything, this observed effect is down to.
"What we can be sure of is that the development of type 2 diabetes is strongly linked to lifestyle, which means that many cases could be prevented by keeping active and eating a healthy balanced diet that is low in fat, salt and sugar with plenty of fruit and vegetables."
This press release is an announcement from the Archives of Internal Medicine
CHICAGO - Individuals who drink more coffee (regular or decaffeinated) or tea appear to have a lower risk of developing type 2 diabetes, according to an analysis of previous studies reported in the December 14/28 issue of Archives of Internal Medicine. A previously published meta-analysis suggested drinking more coffee may be linked with a reduced risk, but the amount of available information has more than doubled since.
By the year 2025, approximately 380 million individuals worldwide will be affected by type 2 diabetes, according to background information in the article. "Despite considerable research attention, the role of specific dietary and lifestyle factors remains uncertain, although obesity and physical inactivity have consistently been reported to raise the risk of diabetes mellitus," the authors write.
Rachel Huxley, D.Phil, of The George Institute for International Health, University of Sydney, Australia, and colleagues identified 18 studies involving 457,922 participants and assessing the association between coffee consumption and diabetes risk published between 1966 and 2009. Six studies involving 225,516 individuals also included information about decaffeinated coffee, whereas seven studies with 286,701 participants reported on tea consumption.
When the authors combined and analyzed the data, they found that each additional cup of coffee consumed in a day was associated with a 7 percent reduction in the excess risk of diabetes. Individuals who drank three to four cups per day had an approximately 25 percent lower risk than those who drank between zero and two cups per day.
In addition, in the studies that assessed decaffeinated coffee consumption, those who drank more than three to four cups per day had about a one-third lower risk of diabetes than those who drank none. Those who drank more than three to four cups of tea had a one-fifth lower risk than those who drank no tea.
"That the apparent protective effect of tea and coffee consumption appears to be independent of a number of potential confounding variables raises the possibility of direct biological effects," the authors write. Because of the association between decaffeinated coffee and diabetes risk, the association is unlikely to be solely related to caffeine. Other compounds in coffee and tea-including magnesium, antioxidants known as lignans or chlorogenic acids-may be involved, the authors note.
"If such beneficial effects were observed in interventional trials to be real, the implications for the millions of individuals who have diabetes mellitus, or who are at future risk of developing it, would be substantial," they conclude. "For example, the identification of the active components of these beverages would open up new therapeutic pathways for the primary prevention of diabetes mellitus. It could also be envisaged that we will advise our patients most at risk for diabetes mellitus to increase their consumption of tea and coffee in addition to increasing their levels of physical activity and weight loss."
Saturday
Here are Dr. Polonsky's 10 etiquette tips for people without diabetes, written from the perspective of someone with diabetes:
- 1 - DON'T offer unsolicited advice about my eating or other aspects of diabetes. You may mean well, but giving advice about someone's personal habits, especially when it is not requested, isn't very nice. Besides, many of the popularly held beliefs about diabetes ("you should just stop eating sugar") are out of date or just plain wrong.
- 2 - DO realize and appreciate that diabetes is hard work. Diabetes management is a full-time job that I didn't apply for, didn't want, and can't quit. It involves thinking about what, when, and how much I eat, while also factoring in exercise, medication, stress, blood sugar monitoring, and so much more - each and every day.
- 3 - DON'T tell me horror stories about your grandmother or other people with diabetes you have heard about. Diabetes is scary enough, and stories like these are not reassuring! Besides, we now know that with good management, odds are good you can live a long, healthy, and happy life with diabetes.
- 4 - DO offer to join me in making healthy lifestyle changes. Not having to be alone with efforts to change, like starting an exercise program, is one of the most powerful ways that you can be helpful. After all, healthy lifestyle changes can benefit everyone!
- 5 - DON'T look so horrified when I check my blood sugars or give myself an injection. It is not a lot of fun for me either. Checking blood sugars and taking medications are things I must do to manage diabetes well. If I have to hide while I do so, it makes it much harder for me.
- 6 - DO ask how you might be helpful. If you want to be supportive, there may be lots of little things I would probably appreciate your help with. However, what I really need may be very different than what you think I need, so please ask first.
- 7 - DON'T offer thoughtless reassurances. When you first learn about my diabetes, you may want to reassure me by saying things like, "Hey, it could be worse; you could have cancer!" This won't make me feel better. And the implicit message seems to be that diabetes is no big deal. However, diabetes (like cancer) IS a big deal.
- 8 - DO be supportive of my efforts for self-care. Help me set up an environment for success by supporting healthy food choices. Please honor my decision to decline a particular food, even when you really want me to try it. You are most helpful when you are not being a source of unnecessary temptation.
- 9 - DON'T peek at or comment on my blood glucose numbers without asking me first. These numbers are private unless I choose to share them. It is normal to have numbers that are sometimes too low or too high. Your unsolicited comments about these numbers can add to the disappointment, frustration, and anger I already feel.
- 10 - DO offer your love and encouragement. As I work hard to manage diabetes successfully, sometimes just knowing that you care can be very helpful and motivating.
Sunday
So you are newly diagnosed as a diabetic and you know that you have to monitor your blood sugar levels, and you know this because the Doctor told you that.
But what you don’t know is what it actually means. This should help.
Blood sugar concentration, (or in reality glucose level), refers to the amount of glucose present in your blood. Normally the blood glucose level is maintained at a reference range between about 3.6 and 5.8 mM (mmol/l). It is tightly regulated as a part of metabolic homeostasis.
WTF? Exactly what does that mean?
metabolic homeostasis basically means keeping (or regulating) the internal systems so as to keep a stable condition.
Mmol/L is the standard unit of measurement and refers to micro moles per litre and you don’t need to understand the chemistry but in case you want to know:
SCIENCE BIT:
Average normal blood glucose levels in humans are about 5mM (mmol/l) this is because the molecular weight of glucose, C6H12O6, is about 180 g/mol). The total amount of glucose normally in circulating human blood is about 3.3 to 7g – because an average human contains about 5 litres of blood. (That is just over a gallon in old money). Glucose levels vary a little during the day, rising after meals for an hour or two by a few grams and are usually lowest in the morning, before the first meal of the day (unless you are a secret midnight snacker).
So, what is this GLUCOSE stuff? Well it is carried by the bloodstream from the intestines or liver to body cells, it is the primary source of energy for body's cells, fats and oils (ie, lipids) being primarily a compact energy store, kind of like a battery. It really doesn’t mean that you should stop eating sugar, it means that you need to better control the type of food that you eat. But that is a separate story.
Failure to maintain blood glucose in the normal range leads to conditions of persistently high (hyperglycemia) or low (hypoglycemia) blood sugar. And that means that your body is not maintaining metabolic homeostasis.
A diabetic fails to maintain metabolic homeostasis and normally is hyperglycaemic and has very high glucose levels and this is often characterised by a constant thirst, with the resultant frequent trips to the loo.
Earlier on in treatment, a diabetic may also start to suffer hypoglycaemic attacks. This is often because the medication has not returned the body to stability and may well be over compensating.
So, at first, you really need to monitor your blood glucose levels, and map it against the food that you eat. That way you can see the effects of what you eat and the medication that you take.
As Alexandr would say ‘Simples’
A group of drugs commonly used for diabetes carry an increased risk of heart problems and death when compared with a different type of diabetes drug, researchers have found.
Their study found that people taking drugs called sulphonylureas are more likely to have heart attacks, heart failure or die, compared to people taking another popular diabetes drug called metformin. Doctors should choose metformin when treating people with diabetes, unless they can't take it or it doesn't work for them, say the researchers.
What do we know already?
If you have type 2 diabetes, it means you have too much glucose in your blood. This can damage your blood vessels, causing heart attacks and strokes, as well as damage to smaller blood vessels in your kidneys, feet, and eyes. Some people with type 2 diabetes control their blood glucose through diet and exercise, but most people need diabetes medicines.
The most commonly used drugs are metformin (brand name Glucophage), and a group of medicines called sulphonylureas. Sulphonyureas include the medicines chlorpropamide, glimepiride (Amaryl), glipizide (Glibenese, Minodiab), tolbutamide, glibenclamide (Daonil, Euglucon), and gliclazide (Diamicron).
Another group called glitazones (also known as thiazolidinediones) are also used. There are two types: rosiglitazone (Avandia) and pioglitazone (Actos).
These medicines all help keep your blood glucose under control, although they work in different ways.
Lately, there's been concern that some of these drugs might increase your chances of having a heart attack or getting heart failure (where the heart can't pump blood efficiently). It's hard to pick up these problems in the clinical studies that are done before drugs are licensed, because they may take a long time to happen, and you need to test very large groups of people to pick up these sorts of differences in risk.
This new study looked at the risks of having a heart attack, getting heart failure, or dying for any reason while taking one or more of the commonly used diabetes drugs. The researchers used figures from a big database of prescribing information, cross-checked with patient records. They compared each type of drug with metformin, because metformin is a well-established diabetes drug that tends to be used first for people with diabetes.
What does the new study say?
The study found that people were more likely to die of any cause, or to get heart failure, while taking a sulphonylurea drug, compared with while taking metformin. They were also more likely to have a heart attack, although this link was not as strong.
It's hard to say exactly how big the difference is. That's because the researchers analysed the results in different ways. Using one set of calculations, the researchers said sulphonylureas were linked to a 60 percent increased risk of death, while using another set, the increased risk was 24 percent.
Of the two glitazone drugs, pioglitazone seemed to be better than rosiglitazone, although the researchers say they need to see more studies to be sure of this. People were less likely to die of any cause while taking pioglitazone, compared with while taking rosiglitazone or metformin. Neither pioglitazone nor rosiglitazone was linked to more deaths or heart attacks than metformin, although rosiglitazone was linked to an increased chance of heart failure. Doctors are already warned not to prescribe rosiglitazone for people at risk of heart failure.
It's important to remember that the study didn't compare the drugs with no treatment. So, it didn't say that people were more likely to die while taking sulphonylureas compared with taking nothing at all. The study may simply show that metformin works better than sulphonylureas.
How reliable are the findings?
The good points of this study are that it covered a lot of people (more than 90,000) over an average of 7 years each. Because of the way the data was recorded, we can compare the risks and benefits of treatments as they're actually prescribed, taking account of the fact that people tend to take more than one drug, or move from one drug to another over time.
However, this makes it harder to account for all the different factors that could affect the results. For example, people might only take sulphonylurea drugs after they'd tried metformin, and it hadn't worked well enough for them, or because they have kidney disease (people with kidney disease can't take metformin). That might mean that people who took sulphonylureas were sicker than people who took metformin, so more likely to die of any cause.
Also, the study relies on all the information on the databases being correctly entered at the time. Because this was a 'real world' study, rather than set up by researchers from the start, there's likely to be more human error in terms of recording data than in a clinical trial.
Where does the study come from?
The study was done by a team of researchers based at Imperial College in London, UK. It was published in the BMJ (British Medical Journal). The study was not directly funded by anyone, although some of the researchers received grants from various research programmes.
What does this mean for me?
If you are taking a sulphonylurea drug, the results of the study might sound alarming. But they may be less alarming than they sound. The study doesn't show that these drugs are actively doing you harm. If they reduce your glucose levels, they protect you against potential problems with your eyes, nerve endings, and feet, as well as treating symptoms such as thirst and tiredness.
What the study shows is that they may not be reducing your overall risk of having a heart attack, heart failure, or dying for any other reason, compared with metformin. Previous studies have shown that metformin seems to reduce the chances of having a heart attack or dying in people with diabetes, especially if you're overweight.
Doctors in the UK are advised to prescribe metformin first for patients with diabetes, although they are told to consider a sulphonylurea in some groups of patients. According to national guidelines, sulphonylureas work faster, so may be used when a quick treatment is needed, and may also be more suitable for patients who are not overweight.
What should I do now?
All diabetes medicines protect against the problems you get from having too much glucose in your blood. It's important not to stop taking medicines without talking to your doctor first.
If you have diabetes and you haven't been treated with metformin before, it may be worth discussing this with your doctor, especially if you're overweight.
Friday
Mind you, quite please I am not taking it at the moment I am on Metformin and Vildagliptin, how long before they say that vildagliptin causes problems and withdraw that?
There is a story in the NHS here, and it has links to the daily telegraph and Daily Mirror stories.
Sunday
From Diabetes Health
Q & A: How To Lower Your Blood Sugar When It's Over 200 mg/dl
Q: How do I lower my blood sugar when it goes over 200 mg/dl? I have type 2 diabetes.
A: An excellent question, but a complicated one to answer. Your doctor or nurse educator should be contacted whenever your blood sugar runs consistently higher than 250 mg/dl for more than two days. When a person with type 2 diabetes encounters a high blood sugar, the strategy used to bring it down will vary from individual to individual. This is because of differences in treatment involving diet, exercise, and medication. It will also depend upon the guidelines for glucose control that you and your doctor have mutually agreed upon.
When high blood sugars do occur, there are a number of strategies that can be employed to lower the glucose level back down to a normal range. These might include:
1) Eating less food at the next meal, eliminating a snack, and/or eating foods with a lower glycemic index.
A general rule of thumb to follow is to eliminate 15 grams of carbohydrate (the amount in one starch exchange, one fruit exchange, or one cup of skim milk exchange), which will lower blood glucose by 30 mg/dl. If you test your blood sugar at 182 mg/dl before a meal or snack, then eliminate one starch and one cup of milk at the next meal to bring the glucose value close to 120 mg/dl as a baseline. Although people with diabetes will respond differently to this adjustment, it provides a basic guideline to start with.
For persons with type 2 diabetes who are overweight, the loss of only five to 10 percent of total weight can dramatically improve blood glucose values. Consequently, just cutting calories moderately can achieve better blood glucose control.
Lastly, choosing foods with a lower glycemic index, that is, foods that do not raise blood sugar as quickly or dramatically, can help to bring blood glucose back into a normal range. Some examples of foods with a low glycemic index are dried beans and lentils.
To test the glycemic effect of a food on your system, you will need to do more frequent monitoring. For example, you may want to compare the effect of brown rice versus baked potato by eating equivalent carbohydrate amounts of these foods at dinner and comparing your blood glucose response two hours later. The exact effect will vary from person to person.
2) Increasing activity or incorporating more exercise.
Persons with type 2 diabetes generally respond to increased exercise with a lowered blood glucose value. Simple exercise, such as walking 20 minutes or more per day, can effectively improve glucose tolerance and induce weight loss. Proper exercise can actually be effective enough to lower or completely eliminate the need for medication altogether.
3) Increasing medications, changing medications, and/or administering them more frequently.
Although this is certainly an option, it makes more sense to first address the problem of elevated blood glucose by exercise and cutting back on food. These measures are less costly and have fewer side effects. If they aren't effective, however, a medication change may be indicated. If you are on the minimal dose of oral agents, your doctor might raise the dose or split it into morning and evening doses.
This could also be true for those using insulin. Taking more shots per day does not mean that your diabetes is worse. It may even bring more flexibility into your lifestyle. In fact, a rule of thumb for those on insulin (check with your doctor first before making these adjustments) is to take one unit of regular insulin to lower blood glucose 30 mg/dl. If your blood sugar is 191 mg/dl before a meal, an extra three units of insulin will bring the glucose down about 100 mg/dl.
It is important to note that this rule may change for people who exercise regularly because it will take less insulin to achieve the desired effect. It may also change for those who become ill because they are more insulin-resistant and may need more insulin to achieve the desired effect. The effectiveness of insulin is also dramatically decreased by high blood sugar levels.
4) Using relaxation techniques and behavioral management.
Relaxation exercises, including deep breathing and audio tapes that guide you through deep muscle relaxation, can reduce stress and help you deal more effectively with it. Tapes are available specifically designed to create images of healthiness in diabetic individuals and encourage visualization of improved glucose control. Behavioral management techniques also increase one's overall sense of control over life and self-efficacy, so that diabetes becomes a state of "wellness in the midst of illness." When you are relaxed and in control, your blood glucose values can improve.
5) Treating identified illness and/or infections.
Illness and infection causes a rise in adrenergic hormones, which increase the production of glucose in the body. This extra surge of glucose is part of the healing process, but can upset glucose control. Thus, continuing to take medications despite poor appetite is vital. You may temporarily require more medication during periods of extended illness. Ask your doctor for instructions on dealing with illness.
6) Monitoring on a more frequent basis and/or monitoring other parameters.
When your blood glucose values exceed the target ranges established by you and your doctor, monitoring should be done every two hours until your blood glucose returns to normal. This gives you an opportunity to treat and adjust blood glucose as soon as possible, rather than waiting until your next doctor visit or next meal (which might be four or five hours later). It also tells you whether or not what you are doing is helping to bring the blood glucose down. Another step to take if your blood sugar is over 250 mg/dl would be ketone checks (done by urine dip stick or via a fingerstick to measure betahydroxybutyrate, an acid). Testing ketones hourly until they disappear is recommended.
7) Increasing consumption of sugar-free fluids.
Often, poor hydration accounts for the concentration of sugar in the blood. All people (with diabetes or not) should drink two to three quarts of sugar-free fluids per day. When glucose is elevated, drinking helps to dilute it. Also, drinking fluids is filling, decreasing the possibility of overeating.
People with heart disease who take diuretics and those with renal (kidney) complications may need to be on restricted fluids. Check with your doctor and/or dietitian if you fall into these special categories.
To combat high blood sugars, the most important strategy is prevention. Prevention of high blood sugars is usually possible with frequent and consistent monitoring. If you have awareness of your usual glucose response patterns to foods and exercise, it will be easier to plan out your day and prevent fluctuations in your blood sugar.
Friday
from Diabetes Health:
World Diabetes Day Is This Saturday, November 14, 2009
Nov 12, 2009
World Diabetes Day is a global awareness campaign that's celebrated every year on November 14. The goal is to encourage action to further the prevention, treatment, and care of diabetes, as well as to support the United Nations Resolution on Diabetes. Landmarks and monuments across the world are lit in blue to create a united voice for diabetes awareness, and diabetes events are held around the globe. As of Monday evening, November 9, the World Diabetes Day website reports that 366 registered diabetes events are scheduled for November 14th, in countries ranging from Saudi Arabia to Argentina to Morocco. In addition, 623 monuments are being lit in blue around the globe. More are sure to be added to the list as the day draws closer and closer.
The U.N. Resolution on Diabetes focuses world attention on the need to stop the diabetes epidemic through urgent action. Governments need to promote low-cost strategies that alter diet, increase physical activity, and modify lifestyles in order to reverse the diabetes tide. According to the California Diabetes Program (DIRC) website, "For governments, [World Diabetes Day] is a call to implement effective strategies and policies for the prevention and management of diabetes to safeguard the health of their citizens with and at risk for diabetes."
Advocacy
The DIRC and the Centers for Disease Control and Prevention (CDC) have suggestions on how communities can help stop the epidemic, including increasing access to affordable healthy food and beverages. We need to advocate to:
- Make healthy food and beverages more available and affordable and restrict availability of less healthy foods and beverages in public places such as schools, government buildings, libraries, and parks
- Increase the number of grocery stores in low-income neighborhoods
- Improve mechanisms for purchasing foods directly from local farms
- Offer incentives to retailers to offer healthy food and beverage options
- Limit advertising of less healthy foods and beverages
- Encourage smaller portion sizes by food vendors
- Discourage consumptions of sugar-sweetened beverages
Educate someone you know about the risks of diabetes
If you are unable to attend a World Diabetes Day event or to witness a monument or building being lit in blue, you can honor the day by educating someone else about the risks of diabetes. They are, according to the DIRC:
- Family history of diabetes
- Increasing age
- Obesity and a sedentary lifestyle
- Ethnicity
- History of diabetes during pregnancy or giving birth to a large baby
- Having high blood pressure or high cholesterol
Everyone can reduce the risk of type 2 diabetes by:
- Exercising
- Eating right
- Losing weight if needed
- Seeing your healthcare provider
- Getting your eyes checked
Sunday
The American Association of Clinical Endocrinologists have bought out new guidelines for the treatment of Type 2. I wonder if the UK guys follow similar guidelines?
Meanwhile whilst exploring other diabetes mellitus solutions beyond Metformin I have stumbled across Berberine, there is this report in the daily telegraph, and a quick google/bing bought up many other references. The dubiously reliable Wiki has a large sectrion on it here and it seems to have tremendous benefits, similar in effect to metformin, but with some added side effect benefits, such as inhibiting Stapphylococcus, fungal infections such as Candida, inhibits cancers such as Breast Cancer, and is a mild anti depressant. Looks like a wonder herb to me, yet a quick trawl of health foods shops doesn't readily find it listed. interesting?
Wonder if I should give it serious consideration and perhaps import it from China?
Thursday
So this is a change in guidelines, I have been on Aspirin since 2006 and I must admit, I bleed like a stuck pig when ever I cut myself (rarely) or do a prick test (frequently). I thought that was good, when I was first diagnosed I used to have the devils own game squeezing the thick gooey blood out of my finger - completely the opposite now.
From a purely non scientific, not knowing what I am talking about, I prefer blood that flows easily !!
read more here
Never a "Duh!" Moment: Study Confirms That Self-Monitoring Improves Patients' Response to Diabetes
Oct 13, 2009
"Self-monitoring blood glucose" (SMBG), a staple in the lives of most people with diabetes who take insulin, involves consistently monitoring and recording blood glucose levels before and after specific activities, such as eating, exercising, sleeping, and taking insulin. By observing the effects of certain foods and activities on their blood glucose levels, patients can learn exactly what works to raise or lower them. Thus, SMBG affords a kind of "fine tuning" approach to diabetes that empowers patients to adjust their medicine, modify their behavior, and manage their disease without always needing expert intervention.
So it's hardly surprising that an international study sponsored by Roche Diagnostics has confirmed that SMBG is a useful tool.
The study, published by SAGE Publications in The Diabetes Educator, looked at the SMBG practice of "paired testing," in which people with diabetes measure their blood glucose levels before and after specific activities to see how modifications in those activities might lead to better BG management. The researchers, located in five far-flung locations-Los Angeles, London, New Delhi, Singapore, and Washington, DC-found that SMBG is helpful to patients because it increases their sense of control and provides nuanced information that allows them to finely hone their diabetes management.
The researchers also looked into the possibility that non-insulin-taking type 2s could benefit from SMBG. Because about 40 percent of type 2 patients are treated with oral drugs or through diet, constant self-monitoring of blood glucose has not been thought to be necessary. Even type 2s who take a combination of oral medications and a daily dose of long-acting insulin are not required to take anywhere near the number of self-administered BG tests that SMBG usually calls for. Given the depth of information and sense of control that SMBG affords, however, even type 2s who do not use insulin may soon hear their healthcare professionals recommending SMBG as part of an aggressive approach to managing type 2.
Saturday
The following came from Diabetes Health and makes an interesting read.
Circadian Rhythm and Blood Sugar Control
Oct 15, 2009
The human body is an amazing machine. The biological clock that ticks inside us to keep the machine running efficiently not only prompts us to sleep and eat on regular basis, but also apparently regulates blood sugar.
Dr. Brian Feldman at Stanford University School of Medicine recently published a study suggesting that a class of steroid hormones called glucocorticoids have a direct effect on a number of genes that affect our biological clock, or circadian rhythm. The circadian rhythm, from the Latin words circa (around) and diem (day), is a 24-hour cycle of biochemical, physiological, and behavioral processes. Glucocorticoids are secreted from the adrenal gland, sometimes at high levels and sometimes at very low levels, depending upon the time of day, when we eat, and the types of food we consume. When blood sugar is lowest, glucocorticoid levels are highest, initiating gluconeogenesis to break down fat in the liver and thereby provide additional glucose to the blood.
Glucocorticoids affect the immune system by up-regulating anti-inflammatory proteins and down-regulating pro-inflammatory proteins. In fact, glucocorticoids are marketed as nasal sprays, which alleviate inflamed nasal membranes, and as asthma inhalers, which reduce inflammation in the lungs. Prednisone, for example, is a prescribed corticosteroid (glucocorticoid) for the treatment of severe asthma or severe allergies. Although it is a valuable treatment option for some conditions, people with diabetes should be especially wary of taking such a powerful steroid because of the fact that glucocorticoids also stimulate gluconeogenesis. The consequent increase in available glucose would be a very serious side-effect for someone whose blood sugar levels are not well-controlled.
While it was thought that glucocorticoids triggered or synchronized the up-regulation and down-regulation of some circadian clock-associated genes, the how's and why's had not yet been well described. Therefore, the first phase of Dr. Feldman's study consisted of applying synthetic glucocorticoids to human and mouse stem cells grown in a dish, to see which genes in the stem cells were activated by the glucocorticoids. The researchers found that glucocorticoids directly activated several of the genes that control the circadian clock.
The next step was to look at how the hormone's control of the circadian clock was associated with other biological processes. Using mice that were genetically engineered to be missing a gene involved in circadian rhythm (Per2; one of the activated circadian clock genes), scientists were able to determine that while glucocorticoids had an effect on glucose homeostasis in normal control mice, there was no effect in mice missing the Per2 gene. This finding suggests that glucocorticoid regulation of circadian rhythm (by way of activating the Per2 gene) is directly involved in glucose homeostasis. Mice lacking the biological clock gene Per2 did not respond normally to glucose homeostasis challenges. These genetically engineered mice also had increased leptin levels as compared to controls. Leptin is a hormone that helps regulate energy expenditure and cycles with the circadian rhythm opposite to the cycle seen with glucocorticoids.
In the study discussion, Dr. Feldman noted that glucocorticoids act "as a synchronization signal to coordinate the circadian rhythm with energy balance. Taken together, our results imply that glucocorticoids regulate glucose homeostasis, in part, through direct control of the circadian clock, which in turn modulates leptin levels."
The study was published online October 5, 2009, in the Proceedings of the National Academy of Sciences (PNAS).
Thursday
 What is up with my body chemistry?
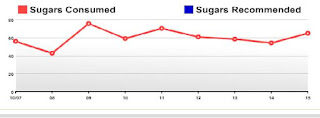
What is up with my body chemistry?My Carbs are well within recomended daily allowance, typically less than 300g per day, usually well below 250:

My Sugars are just as great:
in fact all my figures are good:
| Cals | Fat | Cholest | Sodium | Carbs | Sugars | Fiber | Protein | |
| This week: Click totals for charts! | 9,261 | 239g | 123mg | 5,878mg | 1,201g | 307g | 136g | 471g |
| This month: | 17,273 | 509g | 596mg | 12,933mg | 2,112g | 540g | 238g | 859g |
so why is my blood sugar rising and why do I feel so crap?

Sunday
I am constantly amazed at the benign uses war and space inventions can be turned to. Here is a way forward for quick diabetes indication courtesy of our friends in NASA. I found this on Diabetes Health.
Spyware That Tests for Diabetes?
Oct 9, 2009
MSGI Security Solutions, which "serves the needs of counter-terrorism, public safety, law enforcement, and commercial security," has moved into a new area: diabetes detection. In fact, it has developed a handheld sensor that detects diabetes by measuring the level of acetone in the breath. The device, which employs carbon-based chemical sensors that detect organic vapors, is based upon nano sensors that NASA originally developed to make scientific measurements during space missions.
How does a sensor that detects acetone serve to diagnose diabetes? Because people with diabetes are resistant to insulin or don't produce it at all, their bodies are unable to move glucose from their bloodstream into their cells for energy. When the starved cells call for more glucose, the liver gets into action, converting fat into glucose in a process called gluconeogenesis ("gluco" = glucose; "neo" = new; and "genesis" = production). Gluconeogenesis produces substances called ketones. Ketones break down into three basic compounds, one of them being acetone, which then ends up in the breath.
According to the International Diabetes Federation (IDF), about half of the approximately 246 million people in the world who have diabetes don't know that they have the disease. Early detection would mean that early treatment could be made available. And early treatment, as we know, is absolutely necessary to prevent or delay the complications of diabetes. A simple breath test would go a long way toward simplifying early detection.
Please be aware, however, that this product is still in the prototype stage. MSGI has formed a subsidiary, Nanobeak, which is looking to test the handheld sensor and then license it to Big Pharma. It will then be up to Big Pharma to determine how to market the device to us, the consumers, or to our healthcare providers. (By the way, a nanobeak is a near-field optical head with a beaked metallic plate. Now you know.)
Friday
Critical Actions
There was silence in the room. Then the Sheikh simply said one word, “explain.”
Kahn proceeded to do so. After he had outlined the plan the other three sat and thought and then heads began to nod their agreement and approval.
“So we need to remove any thing that we want to keep from Britain,” Jackson commented.
“Of course, but then you should have done that under the original plan anyway.” Kahn retorted.
“Only if it were at flood level.”
“You would have risked the looting and civil unrest? No, I have had no interests in Britain for a long time, my advice to you all is to do the same. I also do not intend to step foot in the place again. I have no need.”
Giannopoulos looked across at Jackson and then back to Kahn. “I agree, it would be foolishness to retain any property in Britain, or indeed British territories. May I suggest a slight amendment to the plan?”
Kahn nodded.
“I suggest” Giannopoulos continued, “that one hour prior to the detonation we generate a run on every British financial institution. That will complete their destruction.”
“No, absolutely not,” Kahn retorted strongly. “That is totally against our interest.”
“Why not?” from the Sheikh.
“Our intention if you recall. We need to ensure that we have no financial interests remaining in British institutions it is true, that goes with out saying. However everyone of our competitors that has interests in London at the moment of destruction will also face financial loss. That can only be to our advantage and improve our position. May I remind you that our aim is to control the wealth of the world and to do so we need to strengthen the US, and destroy London and seriously weaken Europe.”
“What of your colleagues in the Emirates?” Jackson asked the Sheikh.
“They are already bankrupt as you know, desperately trying to create new ways to make themselves important to the world as the oil runs out. Mohammed is trying to build a holiday resort out of his little sheikdom, but has long since run out of cash. Unfinished skyscrapers line every street, empty shops in the malls and his stupid sand islands are sinking back into the sea. When the oil goes, that will be the end, and the end is a lot sooner than they think. The Persians and Iraqis are just waiting for an excuse to annihilate each other. The plan is above reproach. Once London is gone the only real money and power will lie in the States, and therefore in us.”
“What do you want us to do next?”Jackson asked Kahn.
“London and it’s financial markets are about to be destroyed, all of you need to build them up, make London boom, speed up the recovery, the recession is over, for London. Get your contacts to get as much moved out of Paris and Bonn and into London as possible. Go short, but by 4 weeks, that is the timescale.”
“I have a rather nice collection of Ferraris and Lamborghinis, and a couple of Maybachs in a garage in Mayfair. I think that I shall get them quietly crated and moved.”
“Make sure that they are off the carrier and in your private hands within 4 weeks.”
“Of course, much can be lost in the anarchy that will follow, especially in Europe.”
“Indeed. We also need to raise tensions on the Left Bank and Gaza, if we can get Israel and the Palestinians at each other’s throats and stamp out the Lebanese recovery, that can only aid the process.”
“My area of expertise I think,” the Sheikh volunteered.
“Gentlemen, there is much to do, and we have stayed here longer than expected. We should move.” Kahn drew the meeting to a close, the fourth man had said nothing.
Thursday
One thing that really frustrates people with diabetes mellitus is the biopharma industry's focus on treatments rather than cures. A cure is what the diabetes community wants, not another band-aid. So the existence of a biopharma company that calls itself "CureDM" is promising, and its first product, Pancreate, seems to be on its way to fulfilling that promise.
CureDM started with the information that in most cases, the mass of pancreatic islets drops by 80 percent in type 1 patients and 50 percent in type 2 patients. They also knew from recent research that the adult human pancreas contains an abundance of pancreatic progenitor cells. Like stem cells, progenitor cells have the capacity to differentiate. Unlike stem cells, however, they are not able to become any type of cell. Instead, they differentiate only into their "target" cell, in this case, islets.
In adults, however, pancreatic progenitor cells rarely make the change into islets. Under normal conditions, islets differentiate only during fetal development, when the pancreas is first powering up. When islets do form in adults, it is usually in response to pancreatic injury and stress.
Scientists knew this fact way back before insulin was discovered, when surgeons performed partial pancreatectomies on children with diabetes in hopes of triggering islet regeneration. Rather than hacking off pieces of pancreases, however, CureDM turned to the modern study of genes, called genomics, and proteins, called proteomics. Using these approaches, they were able to identify the key that unlocks the pancreatic progenitor cells, causing them to differentiate into islets. That key is Human proIslet Peptide (HIP), christened Pancreate by CureDM.
HIP is a peptide, or small piece of a protein, made of 14 amino acids (the building blocks of proteins). It is a segment of a large protein that is created by a gene called regenerating islet-derived 3 alpha, or the REG3a gene. HIP stimulates the pathways that cause adult pancreatic progenitor cells to differentiate into functioning islets, fully equipped with alpha, beta, gamma, and delta cells. Because of the scarcity of the REG3a protein after fetal development, CureDM believed that a lack of HIP was the critical element preventing new islet formation, or neogenesis, in adults.
CureDM discovered that the sequence of amino acids in HIP is very similar among many species. When they made a three-dimensional model of the human REG3a protein, they found the HIP part is exposed on the outer surface of the protein, not folded deep within it, making it available to bind with the other proteins that go on to stimulate islet differentiation. And CureDM has successfully stabilized HIP to improve its availability in the body. Recent studies indicate that the dose of HIP required to stimulate islet neogenesis may be 100 times lower than the concentration required by naturally produced HIP.
So far, HIP has been producing some hopeful results. In cultures of human pancreatic ductal tissue, treatment with HIP increases insulin secretion four-fold. In diabetic mice, it triples the number of islets, essentially reversing the disease. Diabetes-related biomarkers normalize in as few as 10 weeks, and diabetic animals no longer need extra insulin after only 21 days of treatment.
CureDM is currently completing the toxicological studies required before filing an Investigational New Drug application, or IND, for Pancreate. An IND is a request for permission from the FDA to administer an investigational drug to humans. The company expects to begin clinical trials in both type 1 and type 2 diabetes in early 2010.